Diabetes management is well suited to use of telehealth, and recent improvements in both diabetes technology and telemedicine policy make this an ideal time for diabetes providers to begin integrating telehealth into their practices. In the post COVID-19 period, patients rightly have concerns to visit crowded hospitals and telediabetes is proving to be a valid alternative. At the same time, on the downside telemedicine can be clinically less reliable with lack of the human touch compounded by the risks of fragmenting health care with various stakeholders, confidentiality concerns and a less favourable revenue model for doctor communities. This article provides specific requirements for effective implementation, and a vision for the future landscape of telehealth to remain within diabetes care providers
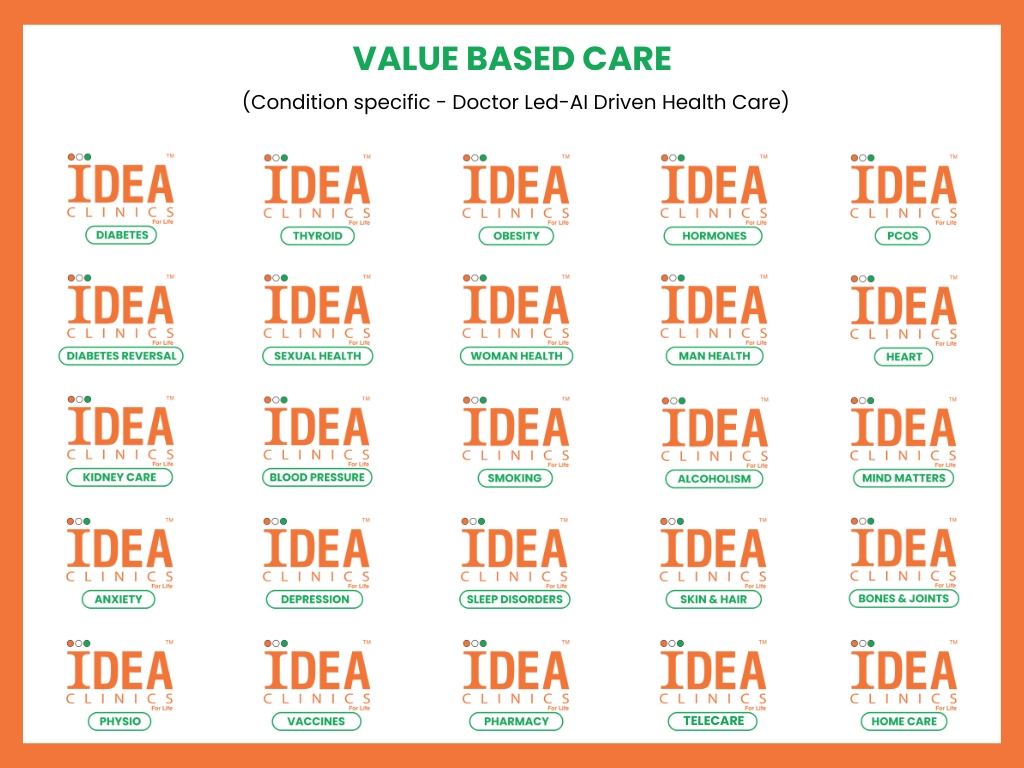
Institute for Diabetes, Endocrinology and Adiposity (Ideaclinics) has audited its patients who accessed its telecare services during the lockdown period. Over 500 teleconsults have taken place during the lockdown period at Ideaclinics. Patients contacted either through phone (Ideacall-8008166166) or via video consults from our websites. Our dedicated telediabetes team comprising of telecallers, diabetes educators, dietitians, home team for phlebotomy and pharmacy have liaised effectively between the patients and doctors, ensured complete 360 degrees diabetes care right from extracting complete medical history, arranging appropriate investigations at home, ensuring home delivery of pharmacy. Various aspects of teleconsults are audited and the responses were as below.









Diabetes is an ideal medical condition for telehealth utilization because it relies heavily on patient self management and use of home medical devices that both generate and capture data. Although diabetes patients have better outcomes with more frequent provider contact, in the present Post COVID-19 era there are certain limitations. Also, Endocrinologists in India are both insufficient in number and sparsely geographically distributed, and frequent clinic visits are difficult to achieve in practice. For these reasons, telehealth has been a focus in diabetes care and part of today’s management relies on use of telephone, electronic health record (EHR) portals, e-mail, text messaging, and others. However, there are concerns for commercial entities promoted by business interests of various pharmacy chains, diagnostics or technology companies to dilute patient care and exploit by inadvertently fragmenting health care for their vested interests. Hence it remains the responsibility of the medical profession to ensure they remain at leadership roles while providing tele services.
Though there are significant technological advances, only a minority of diabetes care providers are routinely adopting these changes as there are concerns about data theft, communication errors, misdiagnoses, and poor outcomes as a result of fragmented healthcare with various stakeholders interrupting the patient journey. Furthermore, although video and teleconsults are now increasingly reimbursed, the doctors have to continue to depend primarily on a fee for service limiting to consultation fee.
One philosophical barrier to telehealth adoption by providers may be the desire for more doctor lead integrated services, encompassing a wide variety of interventions, and with outcome measures. However, it is important to understand that telehealth itself is not an intervention but a care modality. Incorporating telehealth into doctor’s practice adds another tool for communicating with patients and providing the care they need individually.
Practical barriers to the adoption of telehealth by diabetes providers may include uncertainty regarding hardware and software requirements, the process of integrating telehealth into standard workflows in the clinic and EHR, appropriate documentation and reimbursement practices, and determining the optimal frequency and content of telehealth encounters for various patient populations.
In conclusion, for a chronic ailment like diabetes, fragmentation of diabetes care and segregating the patient journey by various piecemeal non medical providers should be discouraged and the doctor community should take up leadership roles and ensure integrated needs of a patient are met. An ideal healthcare should be progressive with a team of expert doctors at the top of a ladder and other junior doctors, nurses, pharmacists, lab technicians, etc., working in close liaison as a team. This should ensure comprehensive, complete and continuous healthcare to patients seamlessly in a cost effective and evidence based approach. Alongside this, at a national level there should be provision for research, data capturing, analytics with newer methods in healthcare being explored to improvise on the existing practices. This can only be achieved when healthcare remains tightly under the supervision of medical professionals at leadership roles. Ideaclinics is one such professional organisation in the preventive healthcare space.